- Home
- >>
- Summary Notes
- >>
- Diseases
- >>
- Obstructive Disease
Asthma Overview
What:
- An immune mediated condition that causes inflammation throughout bronchioles.
- There are many triggers that cause this inflammation
- But all caused by eosinophils – EOSINOPHILIC INFLAMMATION
- They release cytokines
- Cytokines lead to overreactive bronchoconstriction
- Cause an OBSTRUCTIVE SPIROMETRY PATTERN
- A bronchodilator can REVERSE this constriction.
- But all caused by eosinophils – EOSINOPHILIC INFLAMMATION
Who:
Usually diagnosed in children and young adults
Symptoms:
- Wheeze
- SOB
- Non-productive cough
- Symptoms may be episodic in nature
- Diurnal Variability in severity -worst at either night or morning
- May have certain triggers that make symptoms worse (allergens) – pet hair, pollen, dust, occupation (better on holiday?)
Investigations:
- These test various domains of an asthmatics picture – mentioned above. – NEED 2 positive tests to have a diagnosis asthma.
- Investigations depend heavily on the age of the patient.
- Children under 5 are unable to do a true spirometry test usually as they do not breathe in/out fully. – should be assessed every few months after until able:
- Spirometry – testing obstructive picture and improvement with a bronchodilator
- See Spirometry Page for full Discussion on interpretation
- FEV1/FVC – before and after a bronchodilator (salbutamol) – if makes a difference- diagnostic (Bronchodilator Reversibility Test)
- 12% improvement in FEV1 = diagnostic
- Peak Expiratory Flow Rate (PEFR) – testing diurnal variation
- 20% variation throughout set points in day (early, mid-day, evening) suggests diurnal variation. – diagnostic.
- FeNO Test – tests eosinophilic inflammation
- High level of exhaled nitric oxide suggests eosinophilic inflammation – suggests asthma.
- Direct Bronchial Challenge Test– Tests sensitivity of lungs- produces the same reaction as a trigger that exacerbates their symptoms.
- Uses Histamine or methacholine – produced as part of the normal hypersensitivity allergic process in reaction to a patient’s triggers.
- Niche test – only used if still uncertain of diagnosis with other tests being normal
- Spirometry – testing obstructive picture and improvement with a bronchodilator
Management
Management of asthma involves a stepwise progression of measures by adding more drugs- using as little as possible to control symptoms:
Guidelines vary throughout the UK as there is not enough evidence for a single unified treatment path.
Salbutamol is kept throughout all steps of any treatment path to relieve any acute bronchoconstriction.
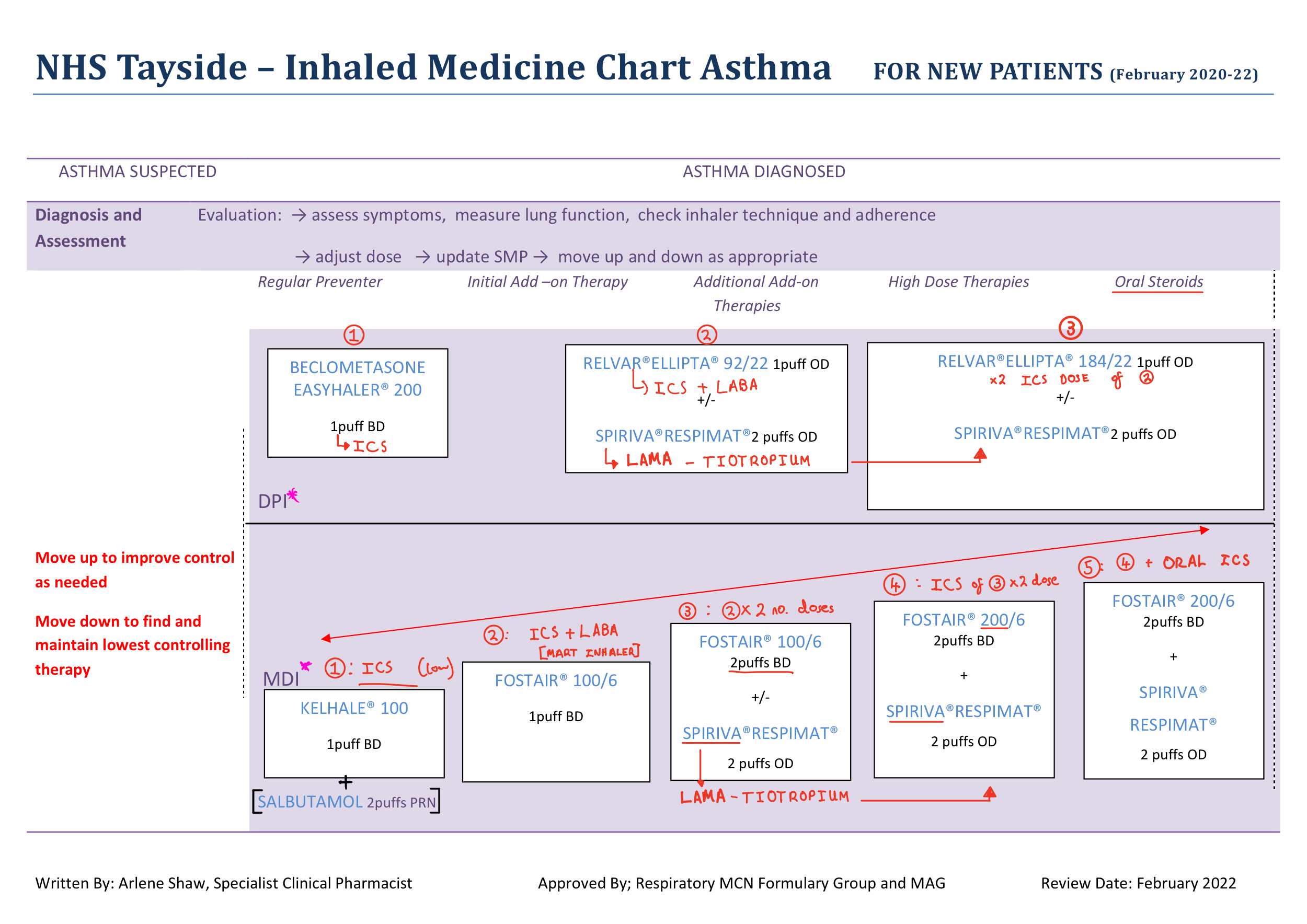
The following are DUNDEE GUIDELINES – used throughout the NHS TAYSIDE TRUST:
- FIRST – SABA (salbutamol) + ICS
- LABA + ICS (low dose) COMBINED INHALER – MART (Maintenance and Reliever Therapy)
- Double number of doses of MART (consider adding LAMA- ipratropium at same time)
- Double dose of ICS in MART + ADD LAMA- tiotropium (if not added)
- Same as 4 but add and ORAL STEROID
This is visualised in the following:
These are NICE GUIDLEINES followed by other NHS trusts throughout the UK. March 2021 Guidlines (reviewed 06/2022):
- FIRST – SABA – Short Acting Beta Agonist as a reliever of symptoms – eg – salbutamol -GIVEN TO ALL
- If frequent use of SABA to control symptoms- Inhaled Corticosteroid (ICS) Added (low dose)
- ADD Leukotreine Receptor Antagonist (LTRA)
- Add LABA if still not controlled – eg – Salmeterol
- (remove LTRA if lack of response)
- Change therapy – MART inhaler (Maintenance and Reliever Therapy) – Combined LABA + ICS (low dose) Inhaler
- (remove individual ICS + LABA )
- Increase Steroid Dose to MODERATE – still using MART (or can change back to individual)
- IF STILL NOT CONTROLLED- can do one of following:
- Increase Steroid Dose to HIGH
- ADD a LAMA
- ADD Theophylline
COPD Overview
What:
- A chronic condition that involves a balance of two factors:
- Emphysema (destruction of alveoli)
- Impairing gas exchange –Irreversible
- Chronic Bronchitis (inflammation of bronchioles)
- A NEUTROPHILIC inflammation
- Causes mucus hypersecretion -> causes mucocilliary dysfuntion -> increased risk of infection.
- Causes smooth muscle spasm – constriction
- PARTIALLY reversible
- Emphysema (destruction of alveoli)
- ONLY comes about as a result of long term, chronic smoking.
Who:
Smokers – usually elderly
Symptoms:
- CHRONIC Symptoms- not episodic with no diurnal variation
- Daily PRODUCTIVE cough (green due to neutrophilic inflammation)
- Progressive breathlessness (gets worse over time) – due to emphysema – so reduced breath sounds
- Breathlessness on exertion
- Frequent infections – Infective COPD exacerbations – Usually viral – antibiotics are of little benefit unless shown to be bacterial through sputum sample.
- Wheeze
Investigations
- Spirometry – mainstay
- Shows an FEV1/FVC of <0.7
- If diagnosis uncertain between asthma and COPD – bronchodilator reversibility testing – COPD less reversible than asthma.
Management
The best thing to manage the disease is SMOKING CESSATION. – stops disease progression completely. – non-pharmacological
NOTE- Inappropriate oxygen prescribing can cause respiratory depression in COPD- Covered in: Common Drugs page
Pharmacological:
- Use a reliever when required – SABA (salbutamol) or SAMA (ipratropium) –ALWAYS
Long term therapy: – Inhaled
- Consider use of just ICS – note increases infection risk
- 2x combo therapy: LABA + LAMA OR LABA + ICS
- 3x combo therapy: LABA + LAMA + ICS:
- If have a severe exacerbation that puts them in hospital
- OR have 2 moderate exacerbations in a year (bad but don’t need admitted)
- OR just still bad on a 2 combo therapy:
RARELY use oral:
-Oral steroid – rarely used
-Oral Theophylline – used more often
Can also give drugs through nebuliser – only if severely disabled by breathlessness.
Progression of Disease
Exacerbation of COPD
This is an Acute-on-chronic worsening of underlying symptoms as a result of an outside factor such as:
- Infection
- Smoking
- Air pollution
This is a common occurrence throughout the course of COPD.
Cor Pulmonale
First results in pulmonary hypertension- leads to Cor Pulmonale (right sided heart failure)
Covered further in: Non-Specific Conditions Page
Sleep Apnoea
- What:
- There are different types of sleep apnoea. The most common is Obstructive Sleep Apnoea (OSA).
- This is due to full upper airway obstruction – with anatomical differences causing the soft palate to completely occlude the pharynx. – Collapse of the upper airway
- Overall this leads to a complete cessation of airflow (apnoea)
- At the point of full occlusion- people with the disease are awoken, multiple times a night, leading to symptoms of fatigue.
- Symptoms
- Chronic fatigue (due to sleep fragmentation) – “Excessive Daytime sleepiness”
- Unrefreshing sleep
- Impaired concentration
- Irritable behaviour
- Morning headache (resolves after a few hours)
- Frequent waking up at night
- Investigation
- Epworth Sleepiness Scale
- Rates chances of falling asleep in 8 situations from 0-3. <10 is normal
- Physical investigation – BP, BMI, Jaw and neck abnormalities
- Sleep Studies done in a specialist clinic – monitors sleep – shows disruption if apparent
- Sleeping pulse oximeter recording
- Epworth Sleepiness Scale
- Management
- CPAP – Continuous Positive Airway Pressure
- A mask worn at night that pumps air through the entire airway. This keeps the airway (including collapsible pharynx) open to allow for complete oxygenation. – A lifelong therapy
- Intra-oral mandibular enhancement – plastic that keeps jaw open- can keep airway open in some
- Surgery – if have large tonsils or have abnormality in bone or soft palate (can reduce) – last line if all else fails.
- CPAP – Continuous Positive Airway Pressure
Cystic Fibrosis and Bronchiectasis
These are 2 obstructive conditions that have been covered further elsewhere: CF extensively on Paediatric Conditions page and Bronchiectasis on Infection page
To summarise these diseases though: they are both very similar in outcome in the respiratory system (bronchiectasis is just in the lungs) .
However differ in how they develop. CF is a GENETIC condition that effects the thickness of secretions throughout the body- in the lungs this results in muco-ciliary dysfunction as these secretions are not able to be cleared by cillia due to their thickness.
Bronchiectasis is due to chronic, repeated damage to the airways (from things like infection) causing scarring of tissue and overall results in airways being widened. This causes muco-cilliary dysfunction that leads to secretions NOT being cleared. Overall leading to a buildup of mucous that leads to an overall NARROWER airway.
- Both of these conditions are characterised by muco-ciliary dysfunction.
- This results in mucous not being cleared
- This results in bacteria trapped in mucous not being cleared
- This results in an increased opportunity for infection
- Chronic infections are a causitive commonality between these diseases as a result.
- This results in bacteria trapped in mucous not being cleared
- This results in mucous not being cleared